Lymphedema can cause painful and unsightly swelling in the arms and/or legs. Though there are varying degrees of lymphedema, Dr. Cheng’s expert microsurgery techniques provide several possible solutions. For patients with Cheng’s Lymphedema late Grade II to Grade IV, and no clear functioning lymphatics shown on indocyanine green (ICG) lymphography images, a vascularized lymph node (VLN) flap transfer is recommended. For patients with more severe cases of lymphedema, such as lymphedema Grade IV, there may be a need for a liposuction or a partial wedge excision one year after the VLN flap transfer.
The choice of the donor site for the VLN flap surgery is based on patient preference, and the availability of sizable lymph nodes at the preferred site. Before the donor site is chosen, Dr. Cheng uses ultrasound images to determine the viability of the lymph nodes. Given these factors, the vascularized submental lymph node (VSLN) flap is the most commonly preferred VLN flap by Dr. Cheng’s patients. Usually, the VSLN flap is transferred to the back of the wrist or to the ankle in accordance with the “pump” mechanism, catchment effect, and natural gravity effect to achieve maximal functional recovery. Though this surgery can provide great relief for painful swelling, the unsightly skin on the wrist may be bothersome to the patient. Fortunately, one-year after VSLN flap transfer surgery it can be removed, leaving a more subtle, linear scar. At this point, the limb previously affected by the lymphedema should be softer and smaller as well.
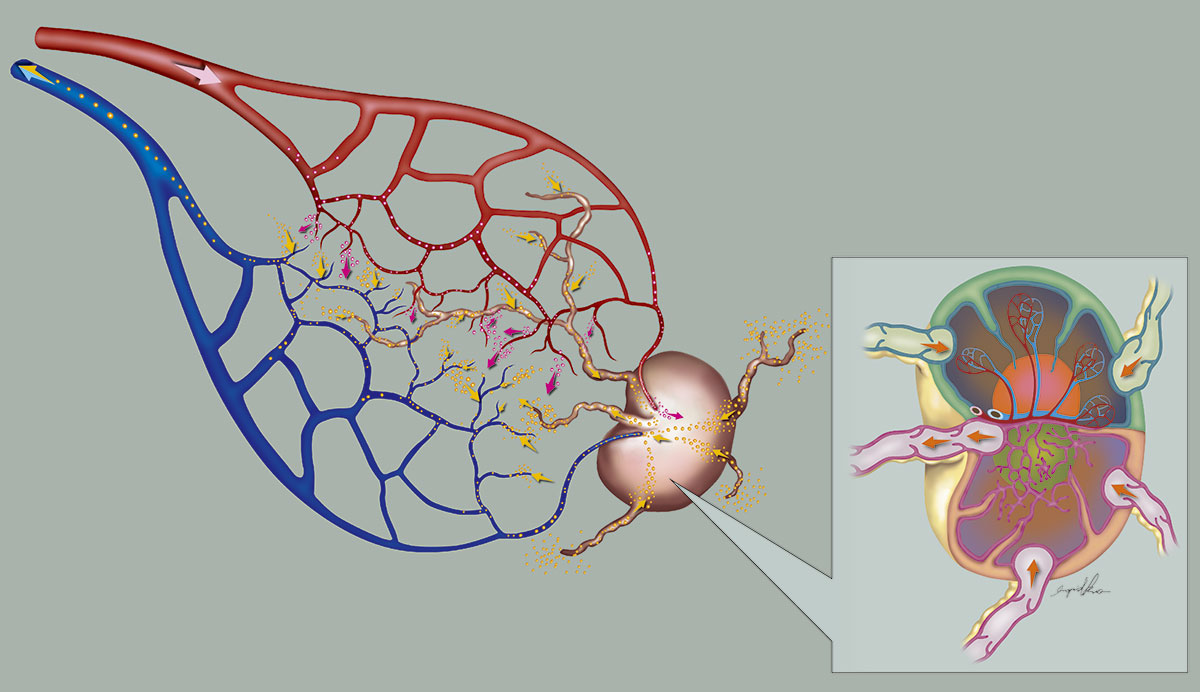 ▲ Intrinsic lymphovenous connections exist within the lymph node flap. These connections are responsible for shunting the lymphatic fluid into the venous system, creating local decompression at the site of vascularized lymph node flap transfer.
▲ Intrinsic lymphovenous connections exist within the lymph node flap. These connections are responsible for shunting the lymphatic fluid into the venous system, creating local decompression at the site of vascularized lymph node flap transfer.
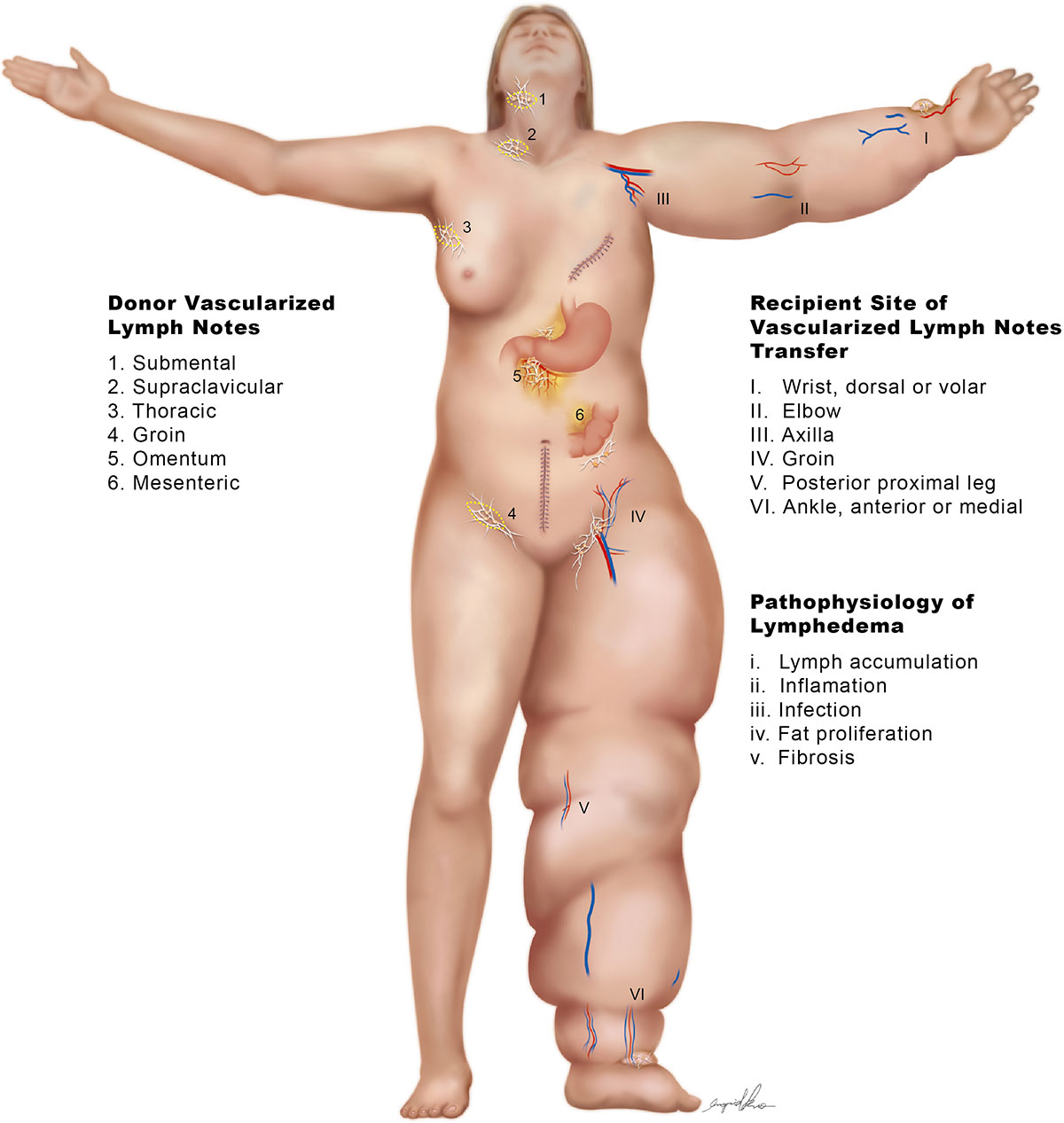
Dr. Cheng’s unique surgical technique can greatly improve the quality of life of patients suffering from lymphedema. By transferring the vascularized lymph node flap to the recipient site, for example to the wrist, Dr. Cheng improves the functionality of the lymphatic system. As a result, the tissue becomes softer, the affected arms and/or legs become smaller and lighter and the patient experiences less cellulitis. This in turn gives the patient an improved cosmetic appearance. In addition, it is important to note that with Dr. Cheng’s superior technique and skills, patients no longer need to wear compression garments post-surgery. Although after VLN flap surgery the initial transferred flap on the wrist is not aesthetically pleasing, one year after the surgery the transferred skin may be removed. Typically done under local anesthesia, this procedure will leave the wrist with a subtle, linear scar instead.
In Cheng’s experience, the success rate of the vascularized lymph node flap is 98%. With an average 18 months of follow-up after VLNT surgery, 90% of BCRL patients show substantial improvement, with an average circumferential difference improvement of 40%. Though patient results vary, in general, post-surgery the affected limb becomes much softer over time; and restriction of daily activities is minimized. After VLN flap surgery patients resume their normal life styles with a boost in self-confidence. A VLN Flap transfer with Dr. Cheng can alleviate lymphedema symptoms, greatly increasing patients’ quality of life.
If you have Breast Cancer Related Lymphedema and would like to know more about the most advanced treatments, contact expert surgeon Dr. Cheng. Internationally recognized as a leading lymphedema specialist, Dr. Cheng can discuss treatment options based on your individual case. Dr. Cheng is a member of the American Society of Reconstructive Microsurgery and has performed numerous VLN surgeries on breast cancer survivors and other lymphedema patients.
Lymphedema is caused by a blockage in the lymphatic system. If the lymph fluid is unable to circulate through the body, it builds-up and causes minor to severe swelling. Typically, lymphedema swelling is seen in the arms and/or the legs, though it can occur is other parts of the body. There are different degrees of lymphedema and some cases can be treated non-surgically. However, for certain types, such as Cheng’s Grade II, III and IV lymphedema, surgery may be the only option to alleviate symptoms and reduce swelling. The VLN flap transfer unblocks the lymphatic system in order to allow the lymph fluid to circulate better, reducing swelling in the affected limb over time. Dr. Cheng has been extremely successful in using this technique to treat moderate to severe cases of lymphedema.
VLN flap surgery with renowned surgeon Dr. Cheng has an excellent success rate. However, the VLN flap surgery is a delicate procedure that requires several follow up appointments after the surgery. These appointments allow Dr. Cheng to carefully measure the circumference of the affected limb or limbs to ensure optimal results. Dr. Cheng will discuss symptom relief with patients, which helps to determine the success of the transferred lymph nodes. Although no compression garments are needed, it is important to attend all follow-up appointments in order to assess progress and determine if any addition physical therapy is necessary.
As an internationally renowned surgeon, Dr. Cheng is an expert in several microsurgery techniques that address lymphedema, including VLN flap surgery. With over a 98% success rate, Dr. Cheng can properly asses your condition and determine what is the best treatment plan. Depending on the grade of lymphedema, Dr. Cheng will recommend the best solution. As a plastic surgeon that specializes in reconstructive microsurgery, Dr. Cheng holds the world record for successfully treating the largest number of lymphedema patients with vascularized lymph node transfers. His unique technique and expert skill enable him to not only diagnose the cause and grade of lymphedema but also propose the best treatment to reduce patients’ symptoms and improve their quality of life.
1. Tc-99m Lymphoscintigraphy Increased Clearance on Static Images
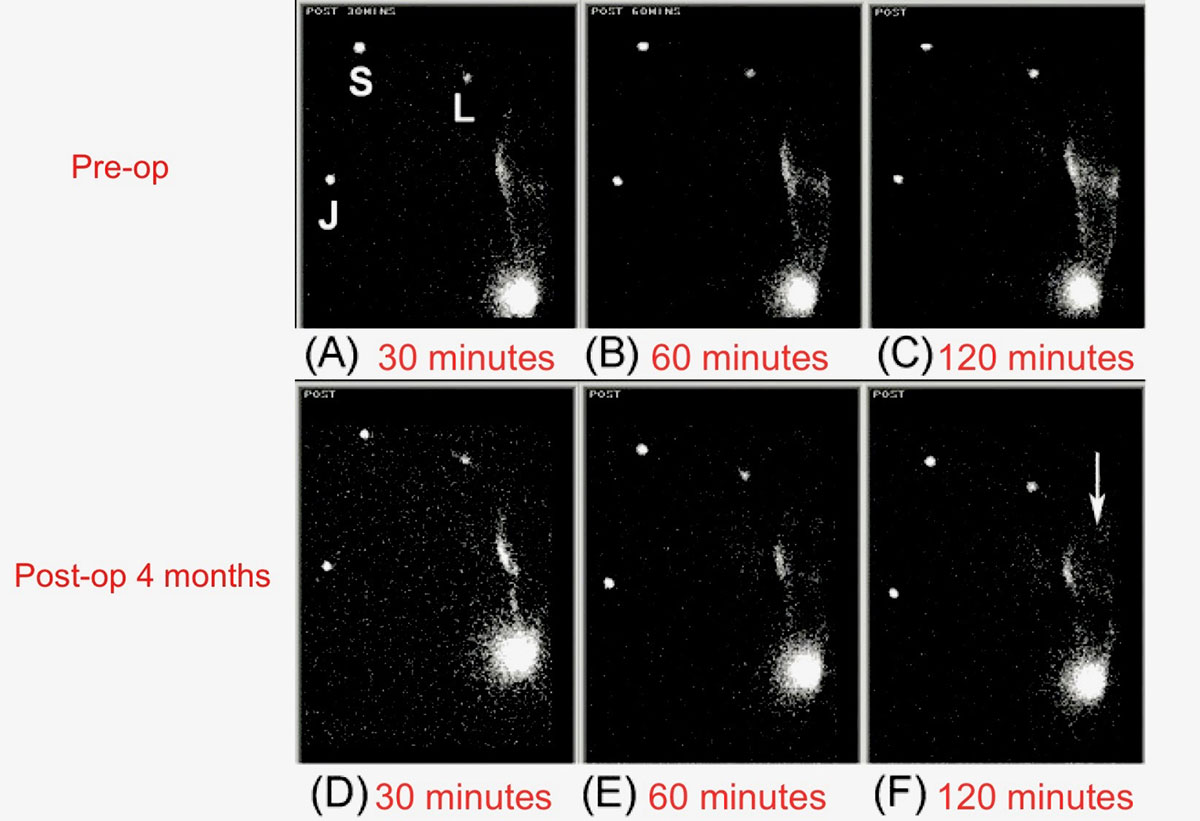 Static views of the same edematous upper limb on posterior view. Images of the upper extremity was taken at 30, 60 and 120 minutes after injection of radio-labelled tracer. Preoperative images (upper row: A-C) and postoperative images (lower row: D-F).In the pre-op images, there is prominent diffuse accumulation of activity shown in the skin of the affected forearm over time. Post-operatively, dermal backflow is less marked in the forearm (D-F) and the radio-labelled tracer has migrated more rapidly to the distal arm (arrow in F).
Static views of the same edematous upper limb on posterior view. Images of the upper extremity was taken at 30, 60 and 120 minutes after injection of radio-labelled tracer. Preoperative images (upper row: A-C) and postoperative images (lower row: D-F).In the pre-op images, there is prominent diffuse accumulation of activity shown in the skin of the affected forearm over time. Post-operatively, dermal backflow is less marked in the forearm (D-F) and the radio-labelled tracer has migrated more rapidly to the distal arm (arrow in F).
2. Vascularized Groin Lymph Node Transfer to Elbow of Post-op Lymphoscintigraphy
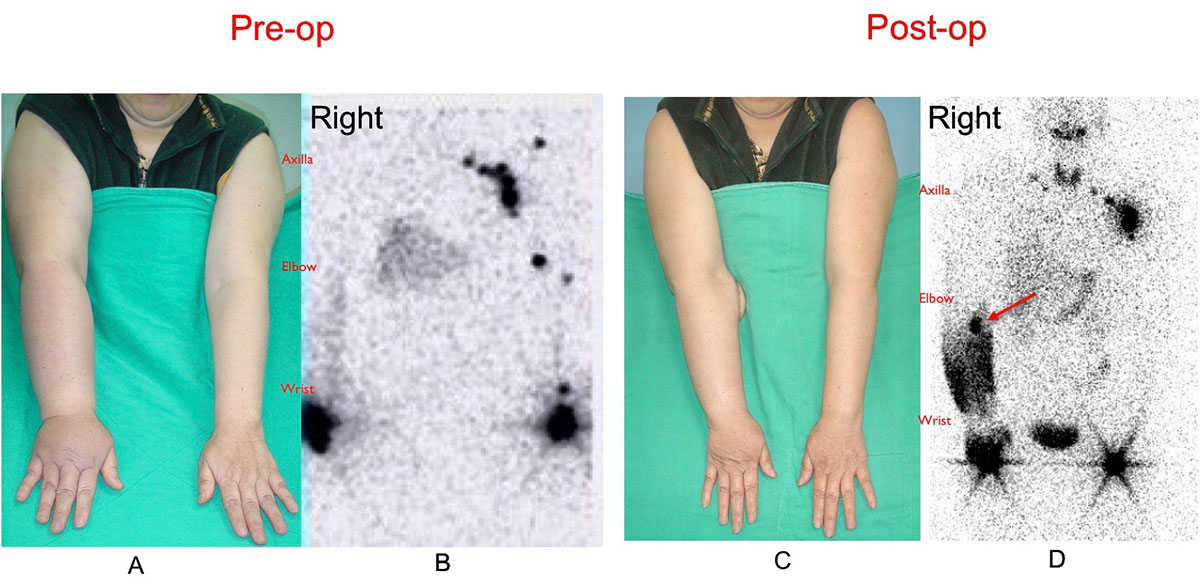 A 68-year-old female patient who was a victim of right upper limb lymphedema underwent vascularized groin lymph node flap transfer to right elbow (A). Preoperative lymphoscintigraphy showed accumulation of Tc-99 in the forearm and absence of right axilla lymph node (B). At a follow-up of 56 months, the patient was satisfied with the softening of left upper limb with a circumferential reduction of 58% above elbow and 40% below elbow (C). Post-op lymphoscintigraphy revealed increased uptake of Tc-99 by the transferred vascularized lymph nodes at the elbow level and less accumulation of Tc-99 in right upper arm (D).
A 68-year-old female patient who was a victim of right upper limb lymphedema underwent vascularized groin lymph node flap transfer to right elbow (A). Preoperative lymphoscintigraphy showed accumulation of Tc-99 in the forearm and absence of right axilla lymph node (B). At a follow-up of 56 months, the patient was satisfied with the softening of left upper limb with a circumferential reduction of 58% above elbow and 40% below elbow (C). Post-op lymphoscintigraphy revealed increased uptake of Tc-99 by the transferred vascularized lymph nodes at the elbow level and less accumulation of Tc-99 in right upper arm (D).
3. Vascularized Submental Lymph Node Transfer to wrist of Post-op Lymphoscintigraphy
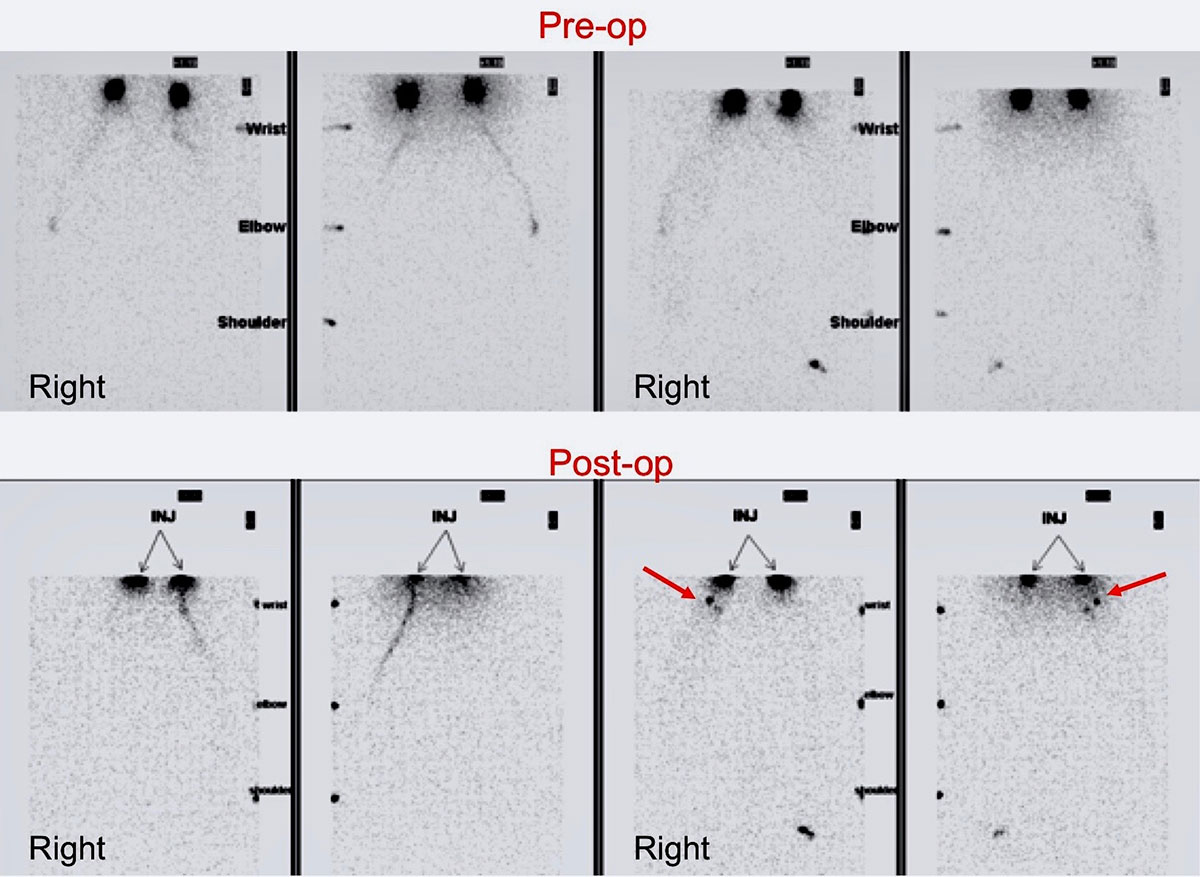 A 52-year-old female patient who was a right upper limb lymphedema underwent vascularized submental lymph node flap transfer to right wrist. Pre-op lymphoscintigraphy showed accumulation of Tc-99 in the forearm and absence of right axilla lymph node. Post-op lymphoscintigraphy revealed increased uptake of Tc-99 by the transferred two vascularized lymph nodes at the wrist level and less accumulation of Tc-99 in right upper arm.
A 52-year-old female patient who was a right upper limb lymphedema underwent vascularized submental lymph node flap transfer to right wrist. Pre-op lymphoscintigraphy showed accumulation of Tc-99 in the forearm and absence of right axilla lymph node. Post-op lymphoscintigraphy revealed increased uptake of Tc-99 by the transferred two vascularized lymph nodes at the wrist level and less accumulation of Tc-99 in right upper arm.
4. Intra-op Image
Data source: Proposed pathway and mechanism of vascularized lymph node flaps. Ito R, Zelken J, Yang CY, Lin CY, Cheng MH. Gynecol Oncol. 2016 Apr;141(1):182-8.

