
As part of the immune system, the lymphatic system helps the body activate a specific immune response against viruses and bacteria. It retains fluid homeostasis in all different compartments of the body. It is made by channels called lymphatic vessels. These collect lymph from all over the body and deliver lymph to the regional lymph nodes or thoracic ducts and then back to the cardiovascular system.
Lymph is a colorless protein-rich fluid that physiologically collects waste products and pathogens. It is present in tissue and transported through the lymphatic system to regional lymph-nodes. The venous flow carries 90% of arterial blood back to the heart and the remaining 10% becomes lymph fluid in the interstitial. Peripheral lymph nodes drain approximately 4-8 liters of lymph fluid per day. The lymphocytes (infection-fighting cells) that reside in the lymph nodes activate a specific immune response against infection.
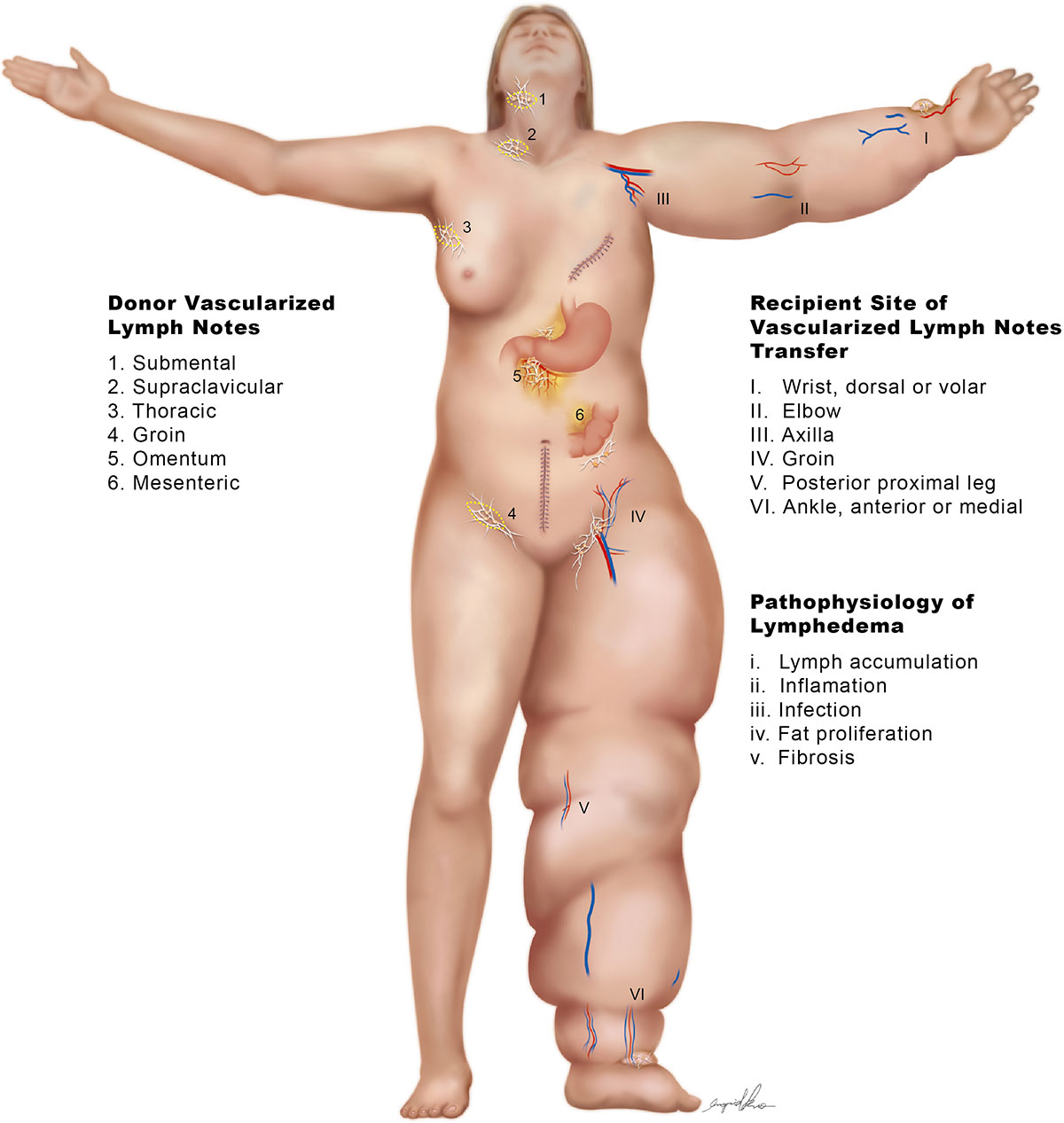
Lymph nodes are bean-shaped organs of the lymphatic system that are distributed widely throughout the body. They are composed by lymphoid tissue enclosed by a capsule of connective tissue. Lymph nodes are major sites of B cells, T cells, and other immune cells. They serve as filters for the blood and provide specialized tissues where foreign antigens and cancer cells can be trapped and exposed to cells of the immune system for destruction. They are typically found concentrated near junctions of the major lymphatic vessels and most prominently found in the neck, groin, and armpits.
The lymphatic system has two important roles: activating the immune response against antigens and transporting lymph fluid. Both functions are important to preserve body homeostasis. When the lymphatic system is compromised by cancer, infections, surgery, trauma, or congenital issues, the affected part of the body is prone to swelling (lymphedema) and recurrent infection due to the faulty surveillance mechanism. The functions of the lymphatic circulation include prevention and resolution of edema, maintenance of interstitial fluid homeostasis, immune trafficking (the regulated transit of antigen-presenting cells to the lymphoid organs), and lipid absorption from the gastrointestinal tract.
One week.
A+ Surgery Clinic has the state of art 42X Mitaka microscope, 3 operation rooms, and professional anesthesiologists, full-time RNs, and 7 private rooms for admission.
Yes. All of our patients are well cared for.
Miffy Lin, Ph.D., chiayumiffy@gmail.com
No. You may check our website: www.lymphedemamicrosurgery.com
Lymphoscintigraphy and ICG are required to make an accurate diagnosis and staging for the treatment, either LVA or VLNT. MRI does not help for the treatment.
Please check platelet count, since the heparin-induced thrombocytopenia and thrombosis is the most common complications post VLNT, specially for those patients with heparin exposure such as the Port-A insertion for chemotherapy.
Surgical record, pathology reports, Lymphoscintigraphy and ICG.
CBC/DC, Chest X-ray, EKG, Lymphoscintigraphy and ICG.
I personally perform the surgery through the entire procedure.
No need.
LVA: 2 hours, VLNT 4-5 hours.
LVA: 2 days, VLNT 5-7 days.
Not much pain immediate postoperatively, most patients do not need intravenous pain killer.
The heparin-induced thrombocytopenia and thrombosis (HITT) is the most common complication post VLNT, about 15 %, especially for those patients with heparin exposure such as the Port-A insertion for chemotherapy. HITT will develop the local pedicle artery or vein thrombosis, which will affect the survival and function of the VLNT. Infection is rare.
See above answer.
The side-to-end lymphovenous anastomosis is the better drainage for extremity lymphedema without wearing compression postoperatively. The lymphatic vessels require contraction to push the lymph from distal to proximal, from dependent site to axilla. If the lymphatic vessels are divided and lost its continuity during end-to-end anastomosis, all the segments of lymphatic vessels will lose their continuity and contraction function, which lost the drainage function eventually.
Yes, one side-to-end LVA at the distal forearm is less invasive, no trauma to other healthy lymphatic vessels. No compression garments are required postoperatively.
Yes.
Yes. Once the lymph has been adequately drained into venous system through side-to-end LVA daily, estimated 500 cc per day, the infection and cellulitis has significantly decreased.
Yes, mainly the infection, swelling, and appearance.
Yes.
Yes.
No countervailing potential risks in side-to-end LVA. The temporary cosmesis in the distal recipient site, the potential HITT in VLNT.
If the ICG demonstrating the lymphatic vessels are available at the forearm.
You may visit the testimonials my patients via Youtube at https://www.youtube.com/watch?v=IlNbv0xZdWQ, and https://www.youtube.com/watch?v=NwCw_SQnAPI.
Dr. Joseph Dayan at Memorial Sloan Kettering Cancer Center.
One year post-operatively.
No. I have quite a few international patients from US, Canada, Rusia, Sweden, Dubai, Saudi Arabic, India, and Iraq.
No.
In my opinion, the side-to-end LVA can cure the early grade lymphedema, and VLNT can cure the late grade lymphedema without wearing compression garments. I think there may be some innovation for the treatment of lymphedema in the next 5-10 years.
Bandage and compression garments are not helping the drainage of lymph in the extremity daily. 10% of arterial blood become the lymph (estimated 500 cc /day in the upper limb) in the interstitial, then the lymph accumulates through the lymphatic vessels to axillary lymph nodes, which continuously drains to thoracic ducts, and to venous system. Bandage and compression garments will affect the contraction of the lymphatic vessels. Although the lymphedematous limb seems not swelling, but the lymphatic vessels will be fibrotic changed quickly.
Exercises including yugo, biking, swimming and golfing within 3 hours each time are helpful for circulations. Lymphatic massage is helpful too. Please remember the lymph production is 10% of the arterial flow. Diet control is good. Arm elevation with one pillow during sleep is good.
Please ask Miffy for the details of the cost of possible procedures.
Please ask Miffy for the details of the cost of possible procedures.
I am not familiar with the BUPA insurance policy.
